What is categorised data?
When a clinician/user of a GP clinical system records clinical data they may, as part of entering the information, identify what type of information they are recording.
For example, where the clinician uses a GP system’s allergy function to record a patient’s allergy information it is explicitly identified in the system as an allergy.
The volume of this categorisation varies between provider systems. For the majority of provider systems, the following types of information are explicitly categorised when they are recorded.
- Allergy
- Appointment
- Consultation
- Demographics
- Diary Entry
- Document
- Flag/Alert
- Immunisation
- Investigation
- Medication and Medical Device
- Problem
- Referral
- Test Request
What is uncategorised data?
There is data that a clinician/user will enter without identifying what type of information they are recording. This information is usually entered as either free text or a combination of clinical code(s), values, qualifiers and text.
For example:
- the clinician records the patient’s resting pulse by recording the resting pulse clinical code followed by a value of the patient’s pulse.
- the clinician records that a patient has a sore throat by recording the sore throat clinical code
- the clinician records that a patient reports being irritable with their family as a piece of free text
Consideration was given to attempting to categorise data using the recorded clinical codes. It was decided not to progress this based on a clinical review of its risks and benefits.
Uncategorised data definition
- Uncategorised data is any item of data in the patient record that does not fit into one of the existing or planned clinical areas defined by GP Connect.
Observation profile
Uncategorised data can contain many different types of clinical information. As the type is not known it is not possible to determine which is the correct FHIR® profile to use for the information. Therefore, uncategorised data will always be contained in an Observation profile.
Qualifiers
Qualifiers are used to refine the meaning of the coded element of the record.
Each provider system supports a different set of qualifiers. However, there are three key qualifiers that are common across all provider systems:
- Laterality - for example, a patient record may have a fracture of the left femur.
- Severity - for example, a patient record may have a severe asthmatic attack.
- Episodicity - for example, this is the patient’s first episode of an asthmatic attack.
The provider system will translate all of the qualifiers included with the clinical code into human-readable text and concatenate them with the text entered by the recorder (placing the qualifiers first) and placing in observation.comment.
Values
Values are any reading or result that is recorded with the uncategorised data. For example, the uncategorised data 50373000 (Body Height) may have a value of 156cm.
Single values
The majority of uncategorised data that contains values will only have a single value. In these cases, the value will be exported in observation.value.
Multiple values
There are cases where an item of uncategorised data may contain multiple values. This happens when:
- there is a single clinical code that describes the uncategorised data as a whole and
- each recorded value in the uncategorised data is described by its own clinical code
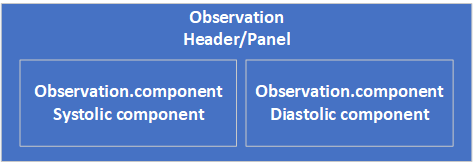
In these cases, each value will be exported in an instance of observation.component.
This approach MUST be used for blood pressure readings where the systolic and diastolic values were taken together.
Hierarchical uncategorised data
There are cases where several pieces of uncategorised data are related to each other in a hierarchical structure.
For example:
- Alcohol Consumption
- Breath alcohol level 15mmol/L
- O/E - spleen just palpable
Where this occurs, the data is supplied in a flattened format with the hierachical information made available to the consumer system if they want to rebuild the hierarchical structure.
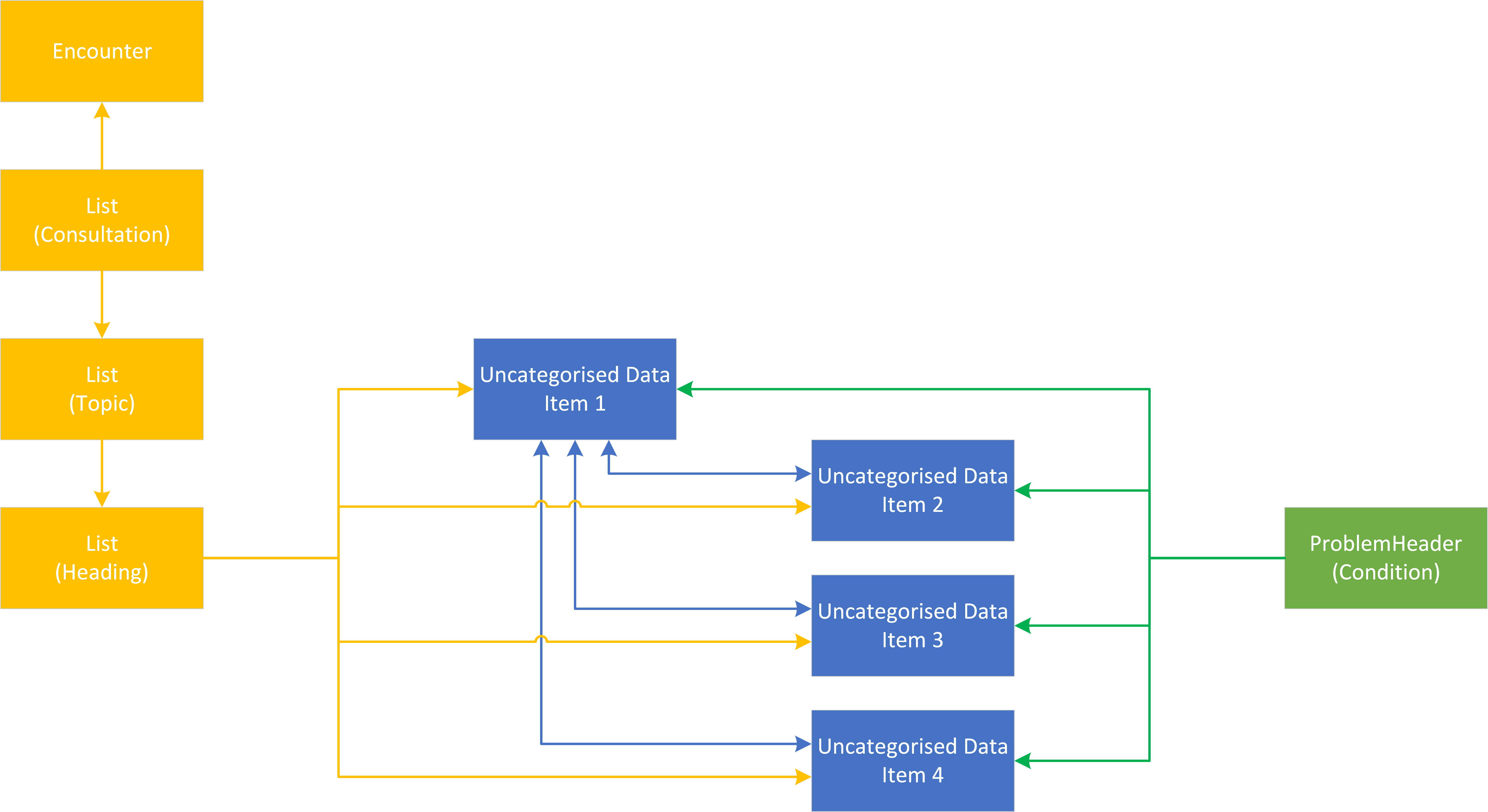
Modeling
Each item of uncategorised data in the hierarchy is recorded in its own observation profile. The structure is represented using the observation.related field.
- The top-level item will contain
observation.related.targetpointing to each of the child items with anobservation.related.typeofhas-member - The child items will contain
observation.related.targetpointing to the top-level item with anobservation.related.typeofderived-from
Note: This follows the same model that will be used to represent Investigations and Pathology.
Consultations and problem
Being in a hierarchy has no impact on the linkage between an item of uncategorised data and a consultation or problem. If the item is recorded in a consultation it will be directly referenced by the consultation. If the item is linked to a problem it will be directly referenced by the problem.
For example, if four items of uncategorised data are recorded under the investigation heading in a consultation with one of the items acting as a parent to the other three items. Direct references to all four items will be populated in the List(Heading) profile. If all four items are linked to a problem then all four items will be populated in the ProblemHeader (Condition) profile.
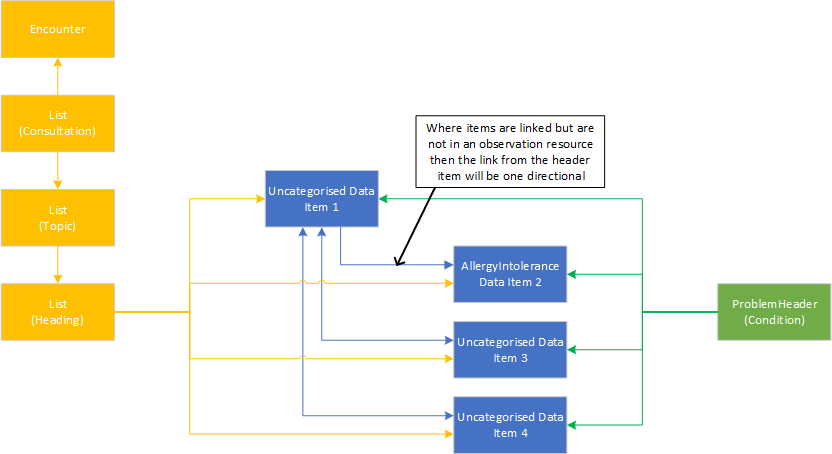
Hierarchical data involving different clinical areas
If the hierarchical data contains items from other clinical areas that are not held in an observation resource, then these should always be included by referencing them from the header observation related element as a ‘has-member’ type. This will mean that, unlike references to other observations, references to these data items will be one directional as illustrated in the diagram below.
Where an item from a different clinical area that is not in an observation resource but is the header element in the native system, then the provider system MUST include them as a child element and create an observation to act as the header with the rubric from the code of the original element in the text field of the codable concept. This MUST be done in accordance with the [uncategorised observation guidelines] and populate the performer and issued elements in line with who recorded the original data and when it was recorded.
Representing blood pressure readings from GP systems
Blood pressure is one of the most common observations that is recorded in GP records. There are over 70 million blood pressures recorded in general practice every year. As this is the case there is a desire to represent the various blood pressure concepts that are recorded in a common format wherever possible. In the majority of cases there are two components that comprise a blood pressure reading regardless of the type of reading. These are a systolic blood pressure reading and a diastolic blood pressure reading. In many cases these are also recorded as a triple with a heading or panel concept. The diagram below demonstrates this structure:
The FHIR vital sign blood pressure profile
This version of GP Connect does not support the ‘vital signs’ aspect of the FHIR specification. However, the way we have represented specified blood pressures is based on the FHIR vital signs blood pressure profile http://hl7.org/fhir/STU3/bp.html. The profile uses a loinc ‘magic code’ to flag certain blood pressures as vital signs. We are not currently using this flag in GP Connect as there is currently no consensus in the UK as to what is/isn’t a vital sign. However, we have done some analysis on how blood pressures are recorded within GP systems in the UK to consider which codes would be appropriate to be sent as a vital sign. Based on this analysis the following codes may in the future be sent as vital signs. They are provided here to enable consuming systems to filter using them if it is desired.
Systolic vital signs codes
Below is the SNOMED binding for systolic codes that represent vital signs in GP systems:
<< 271649006 | Systolic blood pressure (observable entity) |
MINUS
<< 314464000 | 24 hour systolic blood pressure (observable entity) | OR
<< 716579001 | Baseline systolic blood pressure (observable entity) | OR
<< 315612005 | Target systolic blood pressure (observable entity) '
Diastolic vital signs codes
Below is the SNOMED binding for diastolic codes that represent vital signs in GP systems:
<< 271650006 | Diastolic blood pressure (observable entity) |
MINUS
<< 314465004 | 24 hour diastolic blood pressure (observable entity) | OR
<< 716632005 | Baseline diastolic blood pressure (observable entity) | OR
<< 315613000 | Target diastolic blood pressure (observable entity)'
Which codes will be sent using the defined blood pressure structure?
There are many different variations of blood pressure reading or target that are expressed in GP systems in the form of different codes.
Panel/header codes
Any panel or header code that is recorded in conjunction with a recognised systolic or diastolic code MUST be used to populate the code in the main part of the observation. Where the systolic and or diastolic codes are present without a header/panel code then the following codes MUST be used to populate the principle code element: ConceptID - ‘75367002’ DescriptionID - ‘125176019’ Description - ‘Blood pressure’
Systolic codes
The following systolic codes MUST be represented in line with the GP Connect blood pressure structure:
72313002 Systolic arterial pressure (observable entity)
413606001 Average home systolic blood pressure (observable entity)
407554009 Sitting systolic blood pressure (observable entity)
400974009 Standing systolic blood pressure (observable entity)
314449000 Average 24 hour systolic blood pressure (observable entity)
314446007 Average day interval systolic blood pressure (observable entity)
314445006 Average night interval systolic blood pressure (observable entity)
407556006 Lying systolic blood pressure (observable entity)
271649006 Systolic blood pressure (observable entity)
314440001 Average systolic blood pressure (observable entity)
787541000000108 Highest brachial systolic pressure (observable entity)
314448008 Maximum 24 hour systolic blood pressure (observable entity)
314447003 Minimum 24 hour systolic blood pressure (observable entity)
314439003 Maximum systolic blood pressure (observable entity)
314444005 Maximum day interval systolic blood pressure (observable entity)
314438006 Minimum systolic blood pressure (observable entity)
314441002 Minimum day interval systolic blood pressure (observable entity)
314442009 Minimum night interval systolic blood pressure (observable entity)
314443004 Maximum night interval systolic blood pressure (observable entity)
276780008 Left ventricular systolic pressure (observable entity)
276772001 Right ventricular systolic pressure (observable entity)
251070002 Non-invasive systolic arterial pressure (observable entity)
707303003 Post exercise systolic blood pressure response abnormal (finding)
251071003 Invasive systolic arterial pressure (observable entity)
1036551000000101 Non-invasive central systolic blood pressure (observable entity)
Diastolic codes
The following diastolic codes MUST be represented in line with the GP Connect blood pressure structure:
1091811000000102 Diastolic arterial pressure (observable entity)
413605002 Average home diastolic blood pressure (observable entity)
407555005 Sitting diastolic blood pressure (observable entity)
400975005 Standing diastolic blood pressure (observable entity)
314462001 Average 24 hour diastolic blood pressure (observable entity)
314461008 Average day interval diastolic blood pressure (observable entity)
314460009 Average night interval diastolic blood pressure (observable entity)
407557002 Lying diastolic blood pressure (observable entity)
271650006 Diastolic blood pressure (observable entity)
314453003 Average diastolic blood pressure (observable entity)
314459004 Maximum 24 hour diastolic blood pressure (observable entity)
314456006 Minimum 24 hour diastolic blood pressure (observable entity)
314452008 Maximum diastolic blood pressure (observable entity)
314451001 Minimum diastolic blood pressure (observable entity)
314454009 Minimum day interval diastolic blood pressure (observable entity)
314455005 Minimum night interval diastolic blood pressure (observable entity)
314457002 Maximum night interval diastolic blood pressure (observable entity)
314458007 Maximum day interval diastolic blood pressure (observable entity)
174255007 Non-invasive diastolic arterial pressure (observable entity)
250769004 Pulmonary artery diastolic pressure (observable entity)
251073000 Invasive diastolic arterial pressure (observable entity)
276773006 Right ventricular diastolic pressure (observable entity)
276781007 Left ventricular end-diastolic pressure (observable entity)
276774000 Right ventricular end-diastolic pressure (observable entity)
1036571000000105 Non-invasive central diastolic blood pressure (observable entity)
Excluded codes
The following codes MUST NOT be represented using the GP Connect blood pressure structure and should be returned as individual observations:
315612005 Target systolic blood pressure (observable entity)
198081000000101 Ambulatory systolic blood pressure (observable entity)
314464000 24 hour systolic blood pressure (observable entity)
716579001 Baseline systolic blood pressure (observable entity)
814101000000107 Systolic blood pressure centile (observable entity)
315613000 Target diastolic blood pressure (observable entity)
198091000000104 Ambulatory diastolic blood pressure (observable entity)
716632005 Baseline diastolic blood pressure (observable entity)
314465004 24 hour diastolic blood pressure (observable entity)
814081000000101 Diastolic blood pressure centile (observable entity)
Using the List resource for uncategorised data queries
The results of a query for uncategorised data MUST return a List containing references to all Observation resources that are returned.
The List MUST be populated in line with the guidance on List resources.
If the List is empty, then an empty List MUST be returned with an emptyReason.code with the value no-content-recorded. In this case, List.note MUST be populated with the text ‘Information not available’.